— Most people are not experiencing a “good” death.
By Ross Pomeroy
- A new study out of Sweden finds that people who live longer often spend more time undergoing end-of-life care, suggesting that their deaths are more drawn out than people who die younger.
- Medical care at an advanced age often extends life without significantly improving one’s quality of life.
- The study draws further attention to the gap between lifespan and healthspan. In many developed societies, people are living longer but also spending a higher proportion of their lives living in poor health.
Humans are living longer than ever before. Since 1950, global average life expectancy has risen from 47 to 73. This remarkable gain has been won through reducing poverty and eradicating disease, among other humanitarian advances. But in countries whose citizens are now living to advanced ages in the 80s and beyond, a complicated question must now be asked: Are we actually extending life or merely prolonging death?
Extending life or prolonging death?
A team of researchers from the Karolinska Institute in Sweden confronted this query head-on with a study recently published in the American Journal of Public Health. Demographer Marcus Ebeling and his colleagues utilized large public databases to track the course of all deaths of individuals aged 70 and over in Sweden between 2018 and 2020, focusing on patients’ final 12 months. Chiefly, they wanted to know how most elderly individuals die.
Are their deaths short and sudden or long and drawn out? Do they die at home, physically able and mentally sharp until the end? Or do they die in a facility, impaired and care-dependent in their final years, essentially wasting away? Tragically, it increasingly seems to be the latter.
“Two-thirds of all deaths followed a trajectory with extensive elder care utilization throughout the last year of life, and at least half additionally showed extensive medical care utilization,” they found. “Most deaths today do not comply with what is often referred to as a ‘good’ death.”
What constitutes a good death? “Retaining control, being pain-free, having the choice of the place of death, and not having life prolonged pointlessly are principles that have been mentioned, among others,” the researchers wrote.
Ebeling and his colleagues also found that prolonged end-of-life care was increasingly common over the age of 83, Sweden’s life expectancy, suggesting that individuals graced with a longer life are more likely to have a drawn out death, potentially filled with medical procedures and physiological burdens.
Lifespan vs. healthspan
The finding calls further attention to the frequently discussed gap between “lifespan” and “healthspan.” Lifespan is how long someone lives; healthspan is how long someone lives in good health, free from chronic disease and disability. Ideally, they should be nearly equal. In actuality, as human lifespan has rapidly grown over the past half-century, healthspan has not kept up. Analyses suggest a present gap of 10 to 15 years between them in the U.S. That’s more than a decade on average of people living in poor health, often at the twilight of their lives. In keeping with Ebeling’s study, this suggests that most people are in declining health prior to death.
And unfortunately, what a lot of end-of-life care tends to do is boost lifespan, with little benefit to healthspan. Drugs and procedures that treat underlying medical conditions in the elderly are often hamstrung in how much “health” they can truly restore. Ultimately, the best way to boost healthspan and hopefully remain independent until the very end is to prevent debilitating conditions from ever cropping up in the first place. That means eating right, refraining from smoking, drinking alcohol in moderation, maintaining social connections, challenging your mind, and above all, remaining physically active. And it means maintaining these habits even into old age.
The major takeaway is that to give yourself the best chance at a good death, do the things that will help you live a fit life.
Complete Article ↪HERE↩!
How to know when you’re ready to date again after the death of a partner

- If you’re mourning the recent death of a spouse, the idea of dating again may seem impossible.
- But moving forward is an important part of grieving, and dating doesn’t mean you’ve forgotten your late spouse, experts say.
- Crying a lot and wanting to share stories of your spouse are signs you’re ready to date again.
When Mr. Big died in the first episode of “Sex and the City” spinoff “And Just Like That…” Carrie Bradshaw was unsure she’d ever date again.
But as her newly single era unfolds, Carrie finds herself dating, kissing, and sleeping with a string of eligible bachelors who are in their fifties. Throughout it all, Carrie is shown mourning Mr. Big, crying over a photograph of him, making the painful decision to sell the apartment they shared, and wearing Big’s suit jackets as part of her outfits.
Carrie first feels overwhelmed while mourning Big, but as time passes, she regains sight of the life she has ahead of her.
When someone transitions from feelings of intense pain to smaller moments of grief that are mixed in with new experiences, it suggests they’re healing from their loss, Marilyn A. Mendoza, a psychologist who specializes in bereavement wrote for Psychology Today.
“If and when you decide to start dating again, you need to understand that it is possible to be happy in a new relationship even though you are still having thoughts and feelings for your deceased spouse,” Mendoza wrote.
There’s no right or wrong time to start dating again after the death of a spouse, since everyone mourns such a massive loss on their own time, Mendoza said. But there are milestones you can look out for that signal you’re ready for a new romance.
“Try to find meaning in your life and [think about] how you can continue to find meaning while carrying on their legacy here,” Jonathan Singer, a grief specialist at Texas Tech University, told Insider.
You’ve cried a lot or spent days in bed
In order to mourn a life-changing loss like the death of a spouse, you have to allow yourself to feel emotions like sadness, despair, anger, and hopelessness, licensed social worker and therapist Shahem McLaurin previously told Insider.
It can feel overwhelming or impossible to recover in the moment, but crying your eyes out or spending a full day in bed enveloped in sadness are common ways to move through intense grief, even if it feels like the last thing you want to do in the moment. In fact, Sarah Chaves, who lost her father in 2007, wrote that screaming out her intense emotional pain helped her move forward.
As time passes, those feelings should be less acute, allowing you to enjoy parts of life outside of your marriage. But if they don’t dissipate within a year’s time, it could mean you have prolonged grief disorder and should speak with a mental health professional.
“You’ve got to go through rage, but don’t get stuck in it,” Edith Eger, a therapist and Holocaust survivor, previously told Insider.
You want to share stories about your spouse
If you’re dating after the death of your spouse, you’re bound to have sweet or silly memories pop into your head from time to time.
If you get the urge to share one of those stories out loud with a friend or even a date, you should, as it’s an empowering way to dually honor their memory and your strength, Megan Devine, a psychotherapist and grief advocate, previously told Insider.
You still feel grief, but it comes in waves
According to Eger, prioritizing your needs is another sign you’re mourning in a healthy way that’s conducive to dating.
Part of that is realizing you deserve to feel love and support from a romantic partner again, if that’s something you desire. And that desire doesn’t detract from the love you had, and still have, for your late spouse.
When you live by that idea, allowing yourself to have new experiences without your spouse, the grief will no longer feel all-consuming, according to Jacobsen.
Complete Article ↪HERE↩!
4 tips for saying goodbye to someone you love

By Andee Tagle , Sylvie Douglis
Isabel Stenzel Byrnes has spent her entire life practicing goodbyes.
Byrnes, a grief counselor and patient advocate, and her identical twin sister, Anabel Stenzel, were both born with cystic fibrosis, a progressive disease that damages the lungs, pancreas and other organs. It’s a condition that significantly reduced their life expectancy and meant many hospital visits.
But the illness also gave the sisters and best friends a unique perspective. “We both were afraid of death, but we also shared a joint passion for life, knowing that our time could be limited,” says Byrnes. “We knew from an early age that one of us would die first, and we actually practiced that.”
Readying themselves for that final goodbye was a big part of their shared existence – whether that meant making separate friends or entertaining different interests. And yet, when Anabel died in 2013 from cancer, Isabel’s grief loomed large.

“The complete separation of someone as close as my twin was very difficult,” she says, “but I pursued things that made me feel closer to her, and I also strengthened my relationships with friends and family, and that really helped me dig myself out of the hole of grief.”
Now, through her work, Byrnes helps others with the hardships that can come with saying goodbye to loved ones for good.
She shared some advice with Life Kit on the art of thoughtfully saying goodbye – be it a, “See ya later,” a final farewell or one of the many shades of parting in between.
“Recognize the role” of the person you’re parting from
If you want a goodbye to be impactful, offer more than just a generic “Good luck on your future endeavors” or “Thanks for the memories!” Byrnes says no matter how weak or strong a relationship, any goodbye is more meaningful when you take the time to “articulate the value” of that person.
Were they your most trusted colleague? A reliable neighbor? The friend you could always count on for a laugh? Be open and specific about how someone has impacted you, and thank them for the role they played in your life.
Embrace your emotions, then let them go
When processing the grief of separation, Byrnes says it’s important not to judge your emotions. “Saying goodbye naturally evokes really intense emotions,” she says – and that’s OK. If you’re feeling big feelings, that might speak to “the enormity of the loss and the love that [you’ve] experienced.”
Allow those feelings to come — and also, to go. “Because none of us can cry 24/7,” she says.
“We cry, we let it out, and then somehow we end up maybe even talking and laughing. That’s all part of the process.” And then, over time, she says, work to let go of emotions that cost you energy or no longer serve you – things like guilt, anger or envy. Work to remember that person with more love than pain.
Practice goodbye rituals
Not everyone gets the luxury of saying goodbye face-to-face, or in real-time or at all. But Byrnes says saying goodbye is also an internal and symbolic process. Even if you can’t speak directly to the person you’re saying goodbye to, it’s still important to recognize and honor how that person made an impression on you.
Light a candle, write a letter, add an artifact to your ancestral altar or spend a solitary afternoon on the beach. Choose for yourself what ritual best serves you, and then make the time to commemorate that relationship.
Saying goodbye well takes practice
A well-crafted goodbye takes time and care – that’s not always easy. Byrnes says to keep trying anyway. “Authentic, intimate conversation can sometimes be very awkward if you haven’t done that before,” she says. “But really living in the awkwardness, feeling uncomfortable, but doing it anyway is what helps us grow as human beings.”
Though often uncomfortable or difficult, getting familiar with farewells can serve a powerful purpose.
“The other side of the coin of saying goodbye is learning how to love stronger and harder, knowing that a goodbye can come at some point in time.”
Complete Article ↪HERE↩!
Meditating on my death made me feel thrilled to be alive

By Deborah Netburn
On a recent Saturday night, the scene was serene inside Tac-tile Mountain, a small, carefully curated shop in Pasadena. The meditation cushions were laid out on the concrete floor. A sea of white candles was flickering in the window. And then the restaurant next door started blasting “Umbrella” by Rihanna.
The six of us who had gathered inside laughed nervously. We were already excited and a little hesitant. After all, we were there to contemplate our own deaths.
Tac-tile Mountain was hosting “Death Reflections,” a two-hour, $55 workshop led by Marifel Catalig, a trained death doula and breathwork instructor. It had been advertised on Instagram as “a breath guided meditation intended to contemplate death in many forms.” The description ended there, so no one knew exactly what to expect.
Going into the workshop, I hoped that spending an hour meditating on my inevitable demise would ease my fear of dying. What I didn’t anticipate is that I would walk out feeling profoundly grateful for all the ordinary, messy, glittering life I’ve been blessed to live so far.
“What I have been seeing for 15 years now is that knowing one has to die allows one to value life, and feel more grateful for what life allows us to do and enjoy,” she said.
Catalig, 40, greeted us at the door wearing a white blouse and wide-legged jeans, and then asked us to find our seats. After lighting the candles that were placed at the head of each of our cushions, we began with a gentle movement to release the tension of the day, and then focused on our senses — paying close attention to what we could see, hear, taste, feel and smell.
Death meditations are wildly variable. In the Buddhist tradition the practice of maraṇasati, or mindfulness of death, is designed to remind practitioners that death might come as soon as the next morning, the next meal or even the next breath, and encourage them to act accordingly. Another Buddhist practice focuses on a detailed visualization of the body’s eventual decay to help relinquish attachment to the material world.
Catalig once attended a death meditation where participants were wrapped in a white sheet to mimic the shroud they might wear after they die. Another time she led a living funeral workshop where people were asked to write a eulogy for themselves that she read out loud to the group.
The meditation I attended was simpler. The focus was primarily on the type of life review many people undertake before they die.
Accompanied by a playlist of instrumental music that was more evocative than annoying, Catalig asked us to imagine our earliest memories and consider where we were, who was there, what we felt like, what it smelled like and what sounds we heard. We did the same for our early childhood, pre-adolescence, adolescence, early adulthood and on.
As she spoke, memories of the many lives I’ve lived flashed through my mind. Most of them were mundane, but they filled me with a sense of tenderness. There I was playing with a Fisher-Price barn on a green carpet, walking to school in new saddle shoes, riding bikes on the sidewalk with my sister. I saw sleepovers and middle school dances, late summer nights wandering around my hometown, blissfully bored and aimless.
Nobody has lived your life but you. All of your experiences, everything that got you here, that belongs to you.
— Marifel Catalig, breathwork instructor
I saw scenes from my adult life before kids, my life as a new parent, my life with small children and, finally, my life now — my husband, my teenage sons, my colleagues, my friends. All the different and distinct lives I’ve lived.
“Nobody has lived your life but you,” Catalig said. “All of your experiences, everything that got you here, that belongs to you.”
Then the music shifted and she asked us to imagine that we were nearing death. Our eyesight was fading, our hearing becoming more muffled. Food didn’t taste as good as it once did and we were eating less. In my mind I felt myself receding from the immediacy of life — a fog of gray between me and the world. As my experience of the world became more muted, I felt less afraid of leaving it.
Then Catalig had us imagine our last days. Who would visit us? What would they say? And then we pictured our last breath. “What do you want to breathe in?” she asked. “And what do you want to breathe out?”
We imagined hovering above our lifeless bodies, what they would look like, and who would tend to them. For a brief moment, we imagined what might be next.
In a society that rarely encourages reflections on death and dying, many of us respond to our innate fear of death with denial, Testoni said. Carving out time to visualize and imagine our own passing can help us face that fear in a productive way.
“Reflection makes us realize that we are afraid of something we do not know,” she said. “Knowing that we don’t know but we can know a lot is definitely reassuring.”
When the meditation was over, Catalig invited us to share about the experience.
One participant said the meditation helped her reframe the times in her life when she thought she was a bad person. Instead, she saw herself with more compassion. Another participant said she felt that her higher self had been with her all along, and was still with her. This brought her great comfort.
As for me, I walked out of the store in a state of elation. I was less afraid of dying, but mostly I felt so thrilled to be alive.
If you’re curious to try one of Catalig’s death meditations, you can find future offerings on her Instagram page, or contact her through her website breathtodeath.com.
Complete Article ↪HERE↩!
Older people who are homeless need better access to hospice and palliative care

Most people may not wish to devote much time to thinking about their death. However, it’s an unfortunate fact that the entry point into experiences or conversations around death and end-of-life care can happen abruptly.
An unexpected death or a terminal diagnosis can leave people ill-equipped to navigate what often feels like uncharted territory of navigating end-of-life care, bereavement and grief.
The challenging realities surrounding end-of-life care are especially difficult for older people experiencing homelessness. For these older adults, intersectional and compounding experiences of oppression, such as poverty, racial disparities and ageism, create barriers to accessing hospice care.
Misconceptions about hospice care
The need for end-of-life and palliative services for unhoused people will likely continue to grow as the population experiencing homelessness grows and ages.
Currently only 16 to 30 per cent of Canadians have access to hospice and palliative care services, and 34 per cent of Canadians are not clear on who is eligible or who should utilize hospice services. In response, May 7-13 marks National Hospice Palliative Care week, which is aimed at increasing awareness about hospice care in Canada.

The misconceptions about hospice care have had a direct impact on the engagement of services for the public, but also for Indigenous communities and for older adults experiencing homelessness.
Efforts to increase awareness about hospice often neglect the most vulnerable populations. Future efforts must merge education and awareness with intersectionality, which takes into consideration the intersections of inequities that impact unhoused older adults.
Hospice care focuses on addressing the full spectrum of a patient’s physical, emotional, social and spiritual experiences and needs. A common misconception is that hospice is exclusively a location or place where people go to die. Contrary to this notion, hospice is a service that is provided in various settings including within one’s home, long-term care facilities, hospice centres or within a hospital.
End-of-life care
While many Canadians prefer to die at home, older people experiencing homelessness do not have the same opportunities for end-of-life care options, and as a result many unhoused older people die in the hospital or institutional settings.
Family and friends often play an essential role in caring and advocating for a loved one during their end-of-life process. We can only hope to have loved ones by our side during these final stages; however, that is not the reality for many unhoused community members who do not have the option to die at home with loved ones.
Older people experiencing homelessness are especially vulnerable due to limited family or social support networks. Lack of social support can result in unhoused older people feeling isolated and fearful about dying alone or anonymously.
A core focus of palliative care is on easing symptoms and increasing quality of life for people who have a serious or chronic illness, and not solely for those who are dying. Palliative care can be a valuable form of health care for older people experiencing homelessness, as it can offer a tailored approach to managing multiple chronic or terminal illnesses, which are prevalent among unhoused older people.
Palliative care that takes place in a hospital setting can decrease end-of-life care costs by nearly 50 per cent by reducing intensive care unit admissions and unnecessary intervention procedures.
We believe it is valuable to consider that if end-of-life care costs were reduced by using palliative care practices, the cost savings could be used to fund services that directly support unhoused older adults, such as increased affordable housing options.
Aging in the right place
As members of the Aging in the Right Place project research team at Simon Fraser University, we are working to better understand what aging and dying in the right place means to unhoused older adults in two sites providing end-of-life care in Vancouver.
May’s Place Hospice, which is in the Downtown Eastside of Vancouver, provides end-of-life care for community members in that part of the city. May’s Place has created a communal, home-like environment with private rooms, meals provided three times a day, 24-hour nursing care, a smoking lounge and family gathering space.

Another inpatient hospice setting in Vancouver is Cottage Hospice, located in a 1924 heritage building. Patients have a view of the North Shore mountains and are close to the water. Cottage Hospice and May’s place provide the same types of hospice palliative care support, and both care for older patients experiencing homelessness, but serve different populations based on their location and setting, demonstrating that hospice and palliative care is not a one-size-fits all approach.
The Aging in the Right Place project captures the perspectives and lived experiences of older people experiencing homelessness through integrating photovoice interview research methods as well as data collection methods that focused on the hospice setting, the neighbourhood, and experiences of staff who work to support unhoused older people. Photovoice is a method used in community-based research in which participants use photo taking and storytelling to document their own perspectives and experiences.
In the Vancouver area where we work — also known as the land that belongs to the Skwxwú7mesh (Squamish), xʷməθkwəy̓əm (Musqueam) and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) people — and throughout the province, colonization and colonial medical models have had lasting and detrimental impacts on Indigenous knowledge and traditional practices around death and dying for First Nation communities.
One example of these impacts is that current hospice models may not reflect culturally relevant care models. Hospice organizations throughout B.C. should prioritize increasing policy and practice for Indigenous groups to ensure safety and culturally relevant care are implemented. Ensuring accessibility to hospice and palliative care is one step towards dismantling these barriers for Indigenous populations.
B.C. can turn to the Palliative Education and Care for the Homeless (PEACH) service fostered by Inner City Health Associates (ICHA) in Toronto as an example. PEACH is taking a diverse and innovative approach to providing palliative care among the homeless and vulnerable populations, including Indigenous communities and older adults. Innovative and culturally sensitive services such as these, are a step in the right direction to providing better end-of-life care to older adults experiencing homelessness.
It is crucial that we make hospice and palliative care services available to all community members, especially with the aging population and an increase in chronic illnesses throughout Canada.
In addition to supporting community members, hospice and palliative care should focus efforts on tailoring approaches to provide culturally relevant care, increasing staff education about the lived experiences of older people experiencing homelessness, and creating safe and accessible services in B.C. for marginalized communities.
We must actively dismantle misconceptions about the role of hospice and palliative care through education and awareness to facilitate appropriate service delivery and use for diverse populations.
Complete Article ↪HERE↩!
‘It was as if my father were actually texting me’
— Grief in the age of AI

People are turning to chatbot impersonations of lost loved ones to help them grieve. Will AI help us live after we’re dead?
By Aimee Pearcy
When Sunshine Henle’s mother, Linda, died unexpectedly at the age of 72, Henle, a 42-year-old Floridian, was left with what she describes as a “gaping hole of silence” in her life.
Even though Linda had lived in New York, where she worked as a Sunday school teacher, the pair had kept in constant contact through phone calls and texting. “I always knew she was there, no matter what – if I was upset, or if I just needed to talk. She would always respond,” says Henle.
In November, Linda collapsed in her home and was unable to move. Henle’s brother Sam and her sister-in-law Julie took her to urgent care. The doctors found blood clots in her lungs and gave her anticoagulation medication. At first, “nobody seemed to be very concerned about anything,” says Henle. But over the next couple of days, there was a steep decline in her mother’s condition.
A couple of days later, Linda died.
At the peak of the early buzz surrounding ChatGPT in March, Henle, who works in the artificial intelligence industry, made a spur-of-the-moment decision to feed some of the last phone text messages and Facebook chat messages she had exchanged with her mother into the platform. She asked it to reply in Linda’s voice. It had been a few months since her mother had died, and while Henle had previously connected with a local therapist to help her cope with her grief, she found it disappointing. “It felt very cold and there was no empathy,” she says.
She told the chatbot she was upset because she felt like she had made mistakes and that the hospital had also made mistakes, and that she should have been there to advocate for her mother more. The program responded: “Remember the good times we shared. Remember my love for you and let that be your guide. Grieve, yes. Grief is the price that we pay for love. But don’t let it consume you. Remember to live, to love, to enjoy the beauty of this world for you, for me, for everyone who loves you. And sweetheart, remember to take care of yourself. You are so precious and I want nothing more for you to be happy. I’m very proud of you. I love with all my heart and soul.”
Henle was surprised by how much she felt seen by this technology. She also tried using Bard and Bing AI for the same purpose, but both fell short. ChatGPT was much more convincing. “I felt like it was taking the best parts of my mom and the best parts of psychology and fusing those things together,” she says.
While Henle had initially hoped ChatGPT would give her the chance to converse with what she describes as “a reincarnated version of her mother”, she says has since used it with a different intent. “I think I’m going to use it when I’m doubting myself or some part of our relationship,” she says. “But I will probably not try to converse with it as if I really believe it’s her talking back to me. What I’m getting more out of it is more just wisdom. It’s like a friend bringing me comfort.”
For all the advances in medicine and technology in recent centuries, the finality of death has never been in dispute. But over the past few months, there has been a surge in the number of people sharing their stories of using ChatGPT to help say goodbye to loved ones. They raise serious questions about the rights of the deceased, and what it means to die. Is Henle’s AI mother a version of the real person? Do we have the right to prevent AI from approximating our personalities after we’re gone? If the living feel comforted by the words of an AI bot impersonation – is that person in some way still alive?
Chris Cruz was shocked when his father, Sammy, died. He hadn’t thought it was serious when his father was admitted to hospital: he had been in and out of hospital several times before, having struggled with alcohol addiction for years since leaving their Los Angeles home when Cruz was only two years old. “Throughout my whole life there was this aura of danger about him,” says Cruz. “I thought: he’s been through much worse. This isn’t going to get him.” But after two weeks, Cruz received a call from his stepmother. Sammy’s condition had deteriorated. The hospice was asking her for permission to remove Sammy’s life support. Cruz immediately knew what his father would want: “I said yeah, go ahead and do it.”
It took a few weeks for him to fully process that his father was gone. “I was kind of numb from everything leading up to it. He had always had a turbulent relationship with his father, who would frequently make promises that would never materialize. “He tried to see me maybe once every couple of years. We would make plans and then at the last moment he would say that he has some work that he has to attend to,” says Cruz.
Cruz was inspired by an episode of Black Mirror to try to experiment with ChatGPT, but didn’t have high expectations. “I expected it just to not perform, or to give me some kind of response that was obviously created by a program,” he says. He fed ChatGPT old Facebook conversations with his dad and then typed out his feelings. “Just so you know, I’m really sad that you’re not here with me right now,” he wrote. “I’ve done so much since you’ve passed away and I have this great new job. I wish that you could see what I’m doing right now. I think you’d be proud.”
Cruz’s chatbot responded with a positive message of support and encouragement: “I know you’re going to do great things at your new job and your new position. Just remember to keep working hard and go to work every day.” This generic phrasing may not have sounded like his father, precisely, but still, Cruz felt a mix of relief and grief.

While Cruz said that ChatGPT helped provide him with a sense of closure, not everyone in his family understood. “I tried to tell my mom, but she just doesn’t understand what ChatGPT is and she refuses to learn, so it wouldn’t have done anything for her,” he says. When he told his friends, they gave him a half laugh. “They were like: ‘Is this an OK thing to do?’ Because I think it’s still an open question.”
Even before ChatGPT, the question of how to grieve, in a digital world, has become increasingly complex. “The dead used to reside in graveyards. Now they ‘live’ on our everyday devices – we keep them in our pockets – where they wait patiently to be conjured into life with the swipe of a finger,” says Debra Bassett, a digital afterlife consultant.
As far back as 2013, Facebook launched memorial profiles for the dead after receiving complaints from users who were receiving reminders of dead friends or relatives through the platform’s suggestions feature. But some platforms are still struggling to figure out how to memorialize the dead. In May, the CEO of Twitter, Elon Musk, was heavily criticized after tweeting that the platform would be “purging accounts that have had no activity at all for several years”. One user tweeted: “My sister died 10 years ago, and her Twitter hasn’t been touched since then. It’s now gone because of Elon Musk’s newest farce of a policy.”
But until recently, those digital memorials have mostly been places for catharsis. A friend or family member might post a comment on a page, expressing loss or grief, but no one responds. With artificial intelligence, the possibility has emerged for a two-way conversation. This burgeoning field, sometimes called “grief tech”, promises services that will make death feel less painful by helping us to stay digitally connected with our loved ones.
This technology is increasing in use across the world. In 2020, South Korea’s Munhwa Broadcasting Corporation released a VR documentary film titled Meeting You, which features a mother, Jang Ji-sung, meeting her deceased seven-year-old daughter, NaYeon, through VR technology. Jang is in floods of tears as she tells her daughter how much she missed her. Later, they share a birthday cake and sing a song together. It feels both moving and manipulative. Occasionally, it flickers back to reality: Jang is standing in a studio surrounded by green screens, wearing a VR headset.
In China, the digital funeral services company Shanghai Fushouyun is beaming life-like avatars of the deceased on large TV screens using technologies such as ChatGPT and Midjourney – a popular AI image generator – to mimic the person’s voice, appearance and memories. The company says this helps their loved ones to relive special memories with them and allows them to say a final goodbye.
In the US, the interactive memory app HereAfter AI promises to help people preserve their most important memories of loved ones by allowing them to record stories about their lives to share interactively after their deaths.
James Vlahos, the co-founder of HereAfter AI, created a precursor to the platform in 2016, soon after his father was diagnosed with stage 4 lung cancer.
“I had done a big oral history recording project with him, and I had gotten this idea that maybe there would be a way to keep his voice and stories and personality and memories around in a different and more interactive way,” says Vlahos. Together, Vlahos and his father recorded his father’s key memories, including his first job out of college, his experience of falling in love and the story of how he became a successful lawyer.
In 2017, Vlahos wrote about this experience in Wired. After it was published, he heard from other people who were facing loss, and who felt inspired by his creation. He decided to scale the app so that others could use it, leading to the creation of HereAfter AI.
The platform lets people turn photographs and recordings into a “life story avatar” that friends, family and future generations will be able to ask questions to. So a son could ask his mother’s avatar about her first job and hear memories that his real mother had recorded in her actual voice while she was still alive. AI is used to interpret the questions asked by users and find the corresponding content recorded by the avatar creator.
HereAfter ensures that the deceased have given permission for the voice to be used in this way before they die, but ethical questions still loom large over two-way interactive digital personas, particularly on platforms like ChatGPT which can impersonate anyone without their consent. Irina Raicu, the Internet Ethics Program director at Santa Clara University, says that it is “very troubling” that AI is being used in this way. “I think there are dignitary rights even after somebody passes away, so it applies to their voices and their images as well. I also feel like this kind of treats the loved ones as kind of a means to an end,” she says. “I think aside from the fact that a lot of people would just be uncomfortable with having their images and videos of themselves used in this way, there’s the potential for chatbots to completely misrepresent what people would’ve said for themselves.”
A number of technology ethicists have raised similar concerns but the psychotherapist and grief consultant Megan Devine questions whether there really is a line that technology should not cross when it comes to helping people to grieve. “Who gets to decide what ‘helping people grieve’ means?” she asks.
“I think we need to look at the outcome in the use of any tool,” she says. “Does that AI image soothe you, make you feel still connected to her, bring you comfort in some way? Then it’s a good use case. Does it make you feel too sad to leave the house, or make you lean too heavily on substances or addictive behaviors? Then it’s not a good use case.”
Raicu says that the benefits to the user shouldn’t come before the rights of the dead. Her concerns are based on real events. Last year, the Israeli AI company AI21 Labs created a model of the late Ruth Bader Ginsburg, a former associate justice of the supreme court. The Washington Post reported that her clerk, Paul Schiff Berman, said that the chatbot had misrepresented her views on a legal issue when he tried asking it a question and that it did a poor job of replicating her unique speaking and writing style.
The experience can also be unpleasant for these seeking solace. Chris Zuger, 40, from Ottawa, Canada, was also curious to find out whether ChatGPT would be able to imitate his late father, Davor, based solely on the speech patterns of a set of provided prompts.
His father had been hospitalised months previously after a fall. Zuger raced to the hospital when he heard the news, but never got the chance to say goodbye.
“Being brought to the room, I knew very well what the news was going to be. My mother, not so much. Seeing her reaction was devastating,” says Zuger.
Davor, who Zuger describes as a “larger than life character”, was the youngest of 14 children. He was born in a small village in Croatia soon after the second world war. “He was the type of guy who wanted to make sure that his kids had the opportunities that he didn’t. He worked two jobs – just to be able to make sure that we had a roof over our heads and a fridge full of food.”
After going to therapy to help process his grief, Zuger decided to feed in some of his father’s text messages and provided ChatGPT with a description of his father’s speech patterns. Then, he sent a message: “Hey, how’s it going?” He did not keep a record of and can’t remember it word for word, but he remembers that it scared him.
“It was as close as I could figure as if my father were actually texting me,” he says. But it was also a painful reminder that his father was really gone. “It’s not a text from him on my phone. He’s not across the city at his phone typing to me. It’s just prompt, regurgitating back output from its own language model. It was difficult to see the messages while knowing they were not real.”
If his father had known his son had used ChatGPT to recreate his conversations, says Zuger: “He would have thought it was wild and then asked me how to use it. He would have had fun with it. It probably would have got him off Facebook.”
Bassett, who advises technology companies on their treatment of the deceased, refers to the dead whose digital likenesses are manipulated to perform in ways they may not have while alive as digital zombies. Famous examples include Tupac Shakur and Michael Jackson, who have both been digitally recreated to perform live on stage at concerts years after their deaths.
To prevent people from being recreated with technology against their wishes, Bassett presents the idea of a digital do-not-reanimate (DDNR) order – inspired by the physical do-not-resuscitate (DNR) order, which could be part of a person’s will. Vlahos also emphasizes that enthusiastic consent from the deceased should be a requirement for using this technology. He says that one of the biggest challenges that he faces is that many people don’t realize that they want to use this technology until it’s too late for content to be obtained and the required information provided. “It’s something that people kind of think can be put off for another day,” he says. “And then that day doesn’t come. We get a lot of inquiries from people saying that a relative has already died, and asking if we can do something for them. And the answer is no.”
In the future, however, some element of digital afterlife may prove impossible to avoid, whatever our wishes, in part because the development of many AI products has outpaced the ethical questions that surround them. “For most of us who live in the digital societies of the west, technology is ensuring we will all have a digital afterlife,” says Bassett. Even if our conversations are not being fed into a chatbot, our online activity is likely to remain online for others to see for years to come after we die – whether we like it or not.
Complete Article ↪HERE↩!
Almost everyone fears death
— But not in the same ways

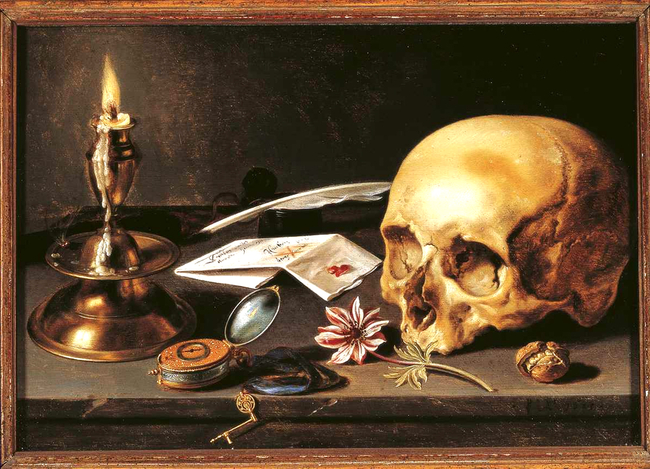
Angel of Death, Evelyn De Morgan, circa 1881
“It is healthy and normal to be afraid of death.”
By Ross Pomeroy
- Fear of death may be the most primal human fear, one we all experience differently.
- People who are older, in committed relationships, physically healthy, and either very religious or not religious at all tend to be less afraid of death.
- When the fear of death becomes extreme and life-disrupting, by far the most effective remedy is cognitive behavioral therapy.
Humans may be the only species fully aware of the inevitability of death. William James, considered by many to be the “father of American psychology,” famously called this fateful knowledge the “worm at the core” of human existence. This metaphorical worm today forms the basis of terror management theory, which proposes that awareness of our mortality, coupled with our self-preservation instinct, produces a primal terror that we constantly struggle to manage. To do so, we often form beliefs and take actions that provide meaning and value that we hope persist beyond our own demise, granting us a semblance of immortality. Other times, we simply cope through escapism or denial.
But just as we all deal differently with the omnipresent foreboding of mortality, so too do we fear death in distinct ways. As Cara Santa Maria, a popular science communicator pursuing a PhD in clinical psychology with a focus on end-of-life care, noted on the Skeptics’ Guide to the Universe podcast:
“Some people are afraid of oblivion. Some people are afraid of dying — the pain, the disability. Some people are afraid of leaving people behind. They’re afraid of leaving things unfinished. They’re afraid of not having a legacy. There are so many different ways that we can be afraid of death.”

Surveys suggest that common fears surrounding death are tied to the prospect of leaving loved ones behind and the dying process itself.
However, certain life choices may ameliorate the fear of death. Being married or in a committed relationship is a significant comfort. Being in good physical health helps, too. This may be because it creates more meaning in life and is broadly linked to better mental health or simply that it grants the perception that the Grim Reaper is farther away. Those on opposite ends of the religiosity spectrum also tend to be less afraid of death. Atheists tend to be more relaxed and “in-the-moment,” while strong believers take comfort in knowing there’s an afterlife and that their life has meaning.
Perhaps most comforting, we tend to grow less afraid of death as we get older. As Jade Wu, a clinical health psychologist at Duke University, writes: “This could be because older people have experienced more of life, so they have less fear of missing out. Or it might be because they have more experience with witnessing and handling the death of others.”

For some, however, the fear of death can be hard to handle, developing into what’s termed thanatophobia.
“It is healthy and normal to be afraid of death, but when we venture into these pathological fears where it becomes all-consuming and it starts to interfere with our activities of daily living, there are things that we can do therapeutically,” Santa Maria said.
By far the most effective remedy is cognitive behavioral therapy. A certified therapist will help a death-fearing client to challenge their anxiety-inducing assumptions about dying and then expose the client to death in ways that will alleviate their fears. Such exposure may include watching movies with scenes that depict the end of life, reading hospice materials, or developing a plan for their own passing.
According to clinical therapist Brittney Chesworth, clients “steadily see death as a normal part of life and not the ‘scary monster in the closet.’”
Complete Article ↪HERE↩!
