By Kavitha Cardoza
Talking about death makes most of us uncomfortable, so we don’t plan for it.
That’s a big mistake, because if you don’t have an end-of-life plan, your state’s laws decide who gets everything you own. A doctor you’ve never met could decide how you spend your last moments, and your loved ones could be saddled with untangling an expensive legal mess after you die.
Betsy Simmons Hannibal, a senior legal editor at legal website Nolo, puts it this way: Planning for the end of life isn’t about you. “You’re never going to really get the benefit of it. So you might as well think about how it’s going to be a lifetime gift that you’re giving now to your parents or your partner or your children. It really is for the people you love.”
Here are some simple, practical steps to planning for the end of life. These tips aren’t meant to be legal or medical advice, but rather a guide to ease you into getting started.
1. Name an executor.
If you’re an adult, you should have a will, says Hannibal. Estate planning is not just for the rich. “It’s not just about the value of what you own. It’s also the feelings that you and your loved ones have about what you own.”
If you own lots of valuable stuff — real estate, trust funds, yachts — you probably need a lawyer. But for most of us, a simple document could do. Your state or county bar associations usually keep a list of lawyers who do this pro bono. Or you could download an online form like Quicken WillMaker & Trust for less than $100. (Full disclosure: Hannibal works for Nolo, which owns Quicken WillMaker & Trust.)
She says the first thing you do is name (in writing) a person whom you trust to take care of everything when you die. In most states that person is called an executor; in some they’re called a personal representative.
Hannibal says it’s a good idea to choose someone from your family. “The most important thing is that you have a good relationship with them — and also that they have a good attention to detail, because it’s a lot of work to be someone’s executor.”
An executor would have to, for example, find all your financial assets and communicate with everyone you’ve named in your will. It’s a big ask, so Hannibal says just be upfront. She suggests asking the person directly, “Would you be comfortable wrapping up my estate when I die?”
2. Take an inventory.
List everything you own, not just things that are financially valuable — such as your bank accounts, retirement savings or car — but also those things that have sentimental value: a music or book collection, jewelry, furniture. Then list whom you want to leave what to.
If you have young children, name a guardian for them. Choose carefully, because that person will be responsible for your child’s schooling, health care decisions and value system.
Hannibal says pets are considered property under the law, so she suggests naming a new owner so that the state doesn’t do it for you.
Digital accounts are also part of your property. This includes social media accounts, online photos, everything in, say, your Google Drive or iCloud, online subscriptions, dating site profiles, credit card rewards, a business on Etsy or Amazon. Hannibal suggests keeping a secure list of all those accounts and the login and password details. Let your executor know where the list is.
Just as you write out specific instructions about your physical belongings, be clear about what you’d like to happen with your online information.
She says it’s better not to have a handwritten will, because proving you wrote it will require a handwriting expert. So keep it simple. Just type out your wishes and have two witnesses watch you sign and date it. Then have them do the same. Hannibal says by signing it, “they believe that the person who made the will is of sound mind, and that’s a pretty low bar.”
You don’t need to file your will anywhere; neither do you need to get it notarized for it to be legally binding. And don’t hide it. Hannibal says just tell your executor where you’ve kept a copy.
Remember that your decisions will change over time. So if you have a child, buy a house or fall out with a family member, update your will.
3. Think about health care decisions.
Your will takes care of what happens after you die. An advance directive is a legal document that covers health care and protects your wishes at the end of your life.
There are two parts to an advance directive. The first is giving someone your medical power of attorney so the person can make decisions for you if you can’t. The other part is called a living will. That’s a document where you can put in writing how you should be cared for by health professionals.
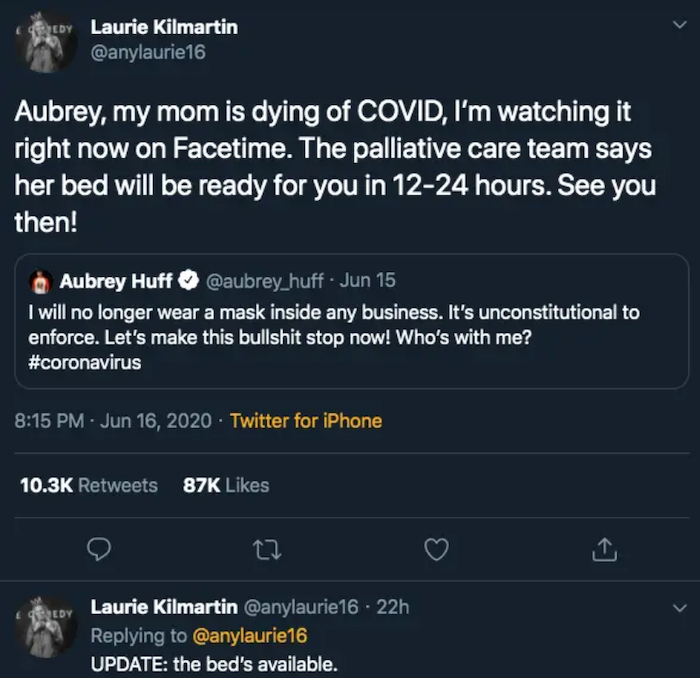
Jessica Zitter is an ICU and palliative care physician in Oakland, California. She says that we’ve become experts at keeping people alive but that quality of life can be forgotten.
She has seen thousands of situations of loved ones making difficult and emotional decisions around a hospital bed. It’s worse when family members disagree about a course of action.
You know the saying “The best time to plant a tree was 20 years ago. The second best time is now”? Zitter says with the coronavirus in the news every day, more people are realizing that these end-of-life conversations are important. “That tree was always important to plant. But now we really have a reason to really, really plant it. … That time is now.”
You may have heard of Five Wishes, which costs $5 and will walk you through choices, or Our Care Wishes, which is free.
4. Name a medical proxy.
Pallavi Kumar is a medical oncologist and palliative care physician at the University of Pennsylvania. Kumar says the most important medical decision you can make is to choose a person who can legally make health care decisions for you if you can’t. This person is sometimes called a medical proxy or a health care agent. Naming the person is the first part of the advance directive.
“Think about the person in your life who understands you, your goals, your values, your priorities and then is able to set aside their own wishes and be a voice for you,” she says. You want someone you trust who can handle stress, in case your loved ones disagree on what to do.
5. Fill out a living will.
After you’ve chosen your medical proxy (and named a backup), you need to think about what kind of care you want to receive. There’s no right or wrong; it’s very personal. The document that helps you do that is called a living will. It’s part two of the advance directive.
A living will addresses questions such as “Would you want pain medication?”; “Do you want to be resuscitated?”; and “Would you be OK being hooked up to a ventilator?”
Kumar says she asks her patients what’s important to them and what their goals are. For some with young children, it means trying every treatment possible for as long as possible, no matter how grueling.
“They would say, ‘If you’re telling me that a chemotherapy could give me another month, I want that month. Because that’s another month I have with my 6-year-old.’ ”
Other patients might want the exact opposite. “They would say, ‘I’ve gone through a lot of treatments and I … feel I’m not having as many good days with my kids. So if the disease gets worse, I want to spend that time at home.’ ”
Kumar says even among patients who are very sick with cancer, fewer than half have had conversations about how they want to die. So talk about your wishes. Once you’ve filled out the advance directive forms, share your decisions with your medical proxy, your loved ones and your doctor.
6. Don’t forget the emotional and spiritual aspects of death.
How you want to die is personal and about much more than just the medical aspect. For some, it’s about being at peace with God; for others, it’s being kept clean. Still others don’t want to be left alone, or they want their pets close by.
Angel Grant and Michael Hebb founded the project Death Over Dinner to make it easier for people to talk about different aspects of death as they eat. “The dinner table is a very forgiving place for conversation. You’re breaking bread together. And there’s this warmth and connection,” says Grant.
Some of the emotional and spiritual questions people talk about are “You were just in a big quake and death is imminent. What are you concerned about not having done?”; “What do you want to be remembered for?”; and “If you could have any musician play at your funeral, who would it be?”
Grant says reflecting on death automatically forces you to think about your life. “That’s the magic of it,” she says.
“We think it’s going to be morbid and heavy. But what these conversations do is they narrow down our understanding of what matters most to us in this life, which then gives us actionable steps to go forward living.”
Grant doesn’t believe a “good death” is an oxymoron. “A good death is subjective, but there are some things that I have heard over and over again for many years at death dinners. … A good death is being surrounded by love, knowing you have no emotional or spiritual unfinished business.”
Complete Article ↪HERE↩!